“Mini-COBRA” Laws in D.C., Maryland, and Virginia
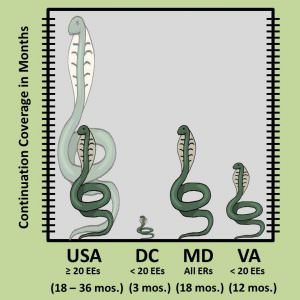 Almost everyone has heard of COBRA: the Consolidated Omnibus Budget Reconciliation Act of 1985. COBRA generally requires that group health plans sponsored by employers with 20 or more employees offer employees and their families the opportunity for a temporary extension of health coverage (“continuation coverage”) in certain circumstances where coverage under the plan would otherwise end. These circumstances include both voluntary and involuntary separation from employment, as well as death, divorce, etc. Continuation coverage under the federal COBRA generally lasts for 18 months – but may last for up to 29 or 36 months in certain limited circumstances.
Almost everyone has heard of COBRA: the Consolidated Omnibus Budget Reconciliation Act of 1985. COBRA generally requires that group health plans sponsored by employers with 20 or more employees offer employees and their families the opportunity for a temporary extension of health coverage (“continuation coverage”) in certain circumstances where coverage under the plan would otherwise end. These circumstances include both voluntary and involuntary separation from employment, as well as death, divorce, etc. Continuation coverage under the federal COBRA generally lasts for 18 months – but may last for up to 29 or 36 months in certain limited circumstances.
Less well known are the state “mini-COBRA” laws that apply to employers with fewer than 20 employees.
D.C., Maryland, and Virginia all have mini-COBRA laws that apply to employers with fewer than 20 employees.
The D.C. mini-COBRA law provides for 3 months of continuation coverage, except in the case of terminations for gross misconduct. The employer is required to provide notice to the employee within 15 days after the date that coverage would otherwise terminate. The employee is responsible for electing coverage and paying the premium within 45 days after the date that coverage would otherwise terminate. D.C. Code § 32-732.
The Maryland mini-COBRA law provides for 18 months of continuation coverage, except in the case of terminations for cause. The employer is required provide an election form within 14 days of request by an employee. The employee is responsible for electing coverage and paying the premium within 45 days after the date that coverage would otherwise terminate. Md. Code, Ins. Art. § 15-409.
The Virginia mini-COBRA law provides for 12 months of continuation coverage, except in the case of terminations for cause. The employer is required provide an election form within 14 days after the date that coverage would otherwise terminate. The employee is responsible for electing coverage and paying the premium within 31 days receiving the notice – but in no event beyond the 60 day period following the date that coverage would otherwise terminate. Va. Code § 38.2-3541.



 Gallery Pl.—Chinatown
Gallery Pl.—Chinatown 